Alzheimer’s Disease Care Services
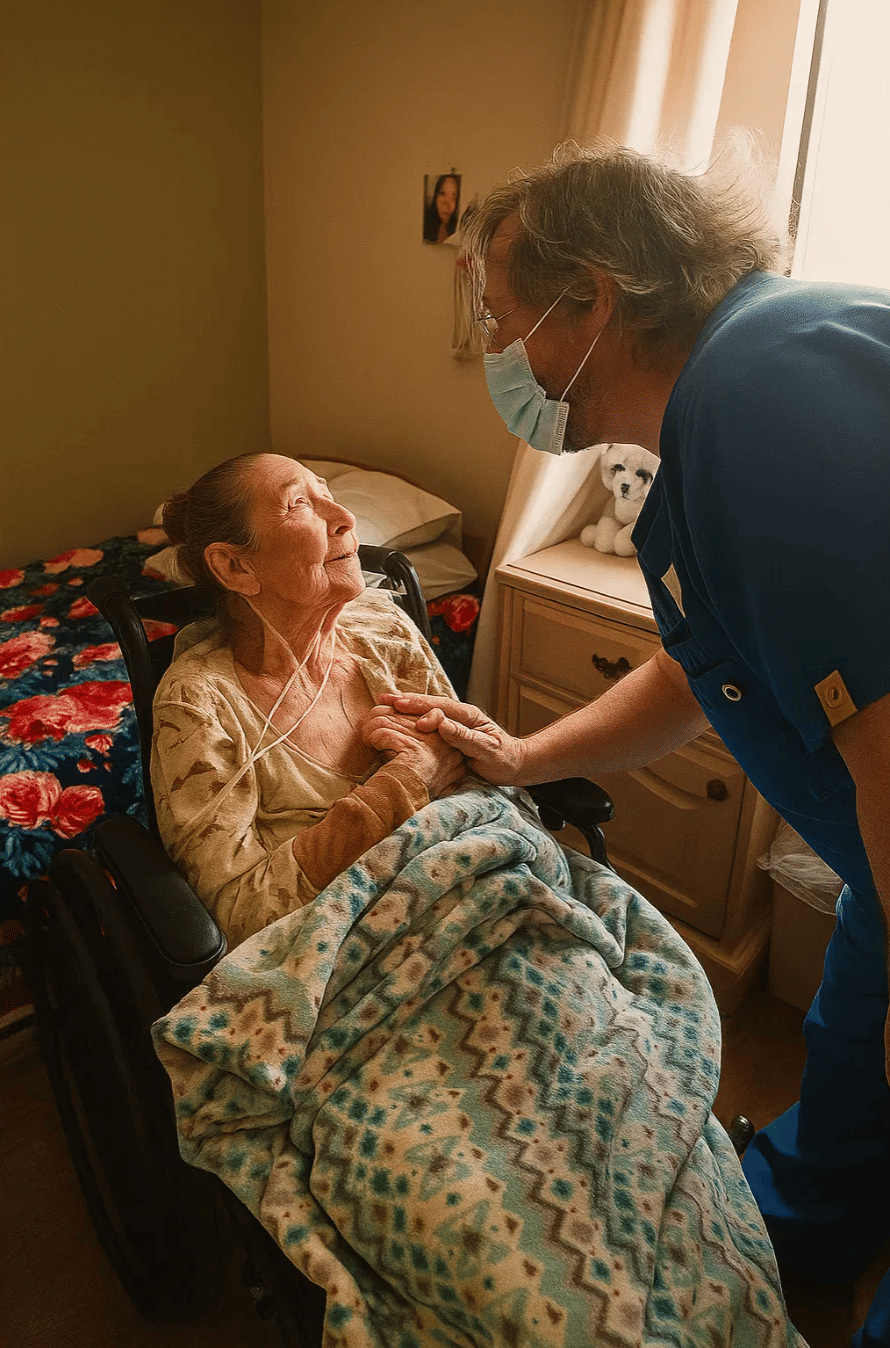
Families facing the challenges of Alzheimer’s disease often reach a moment when specialized support becomes essential, particularly as symptoms progress and daily routines become harder to manage. Compassionate hospice care can ease this transition, providing comfort for the patient and practical support for the family. Alzheimer’s care through hospice focuses on quality of life, symptom relief, and emotional stability, creating a peaceful environment during a difficult stage. Choosing a team that understands the unique progression of Alzheimer’s can transform how families experience this phase, especially when the care plan blends medical guidance, family education, and thoughtful personal attention.


Understanding Alzheimer’s Disease in a Hospice Setting
Alzheimer’s is the most common form of dementia, which means many families arrive at hospice only after a long journey of memory loss, behavioral shifts, and increasing dependence. Hospice care becomes appropriate when cognitive decline reaches the point where communication, orientation, and daily tasks are significantly impaired, often with physical complications developing at the same time. Many caregivers express relief once they learn that hospice does not hasten decline but instead supports comfort, safety, and dignity in a way that typical medical settings cannot always provide.
Alzheimer’s progression often brings challenges related to agitation, wandering, and changes in appetite or sleep routines. Hospice providers step in with strategies that reduce distress for both the patient and the family, making it easier to maintain calm, predictable days. Practitioners who specialize in Alzheimer’s care understand how to adjust interactions, adapt the environment, and anticipate needs to avoid unnecessary discomfort. Support is shaped by the stage of the disease, which ensures that the care plan evolves naturally rather than reacting only when problems arise.
When Alzheimer’s Patients Are Eligible for Hospice
Families often struggle to recognize when hospice becomes appropriate, largely because Alzheimer’s progresses gradually and unpredictably. Eligibility usually becomes clear when the patient’s cognitive function has declined to late-stage levels, which can include limited verbal communication, total dependence on caregivers, or frequent infections and weight loss. Physicians look for a combination of medical markers and functional decline to determine if a person qualifies under Medicare, Medicaid, or private insurance guidelines.
Hospice teams help families document these changes, giving them clarity at a time when uncertainty can feel overwhelming. Many families in Louisiana, Mississippi, and New Mexico find that eligibility becomes easier to understand once they speak with a hospice nurse who can explain how specific behaviors or physical changes relate to the criteria. This guidance offers reassurance that the decision is appropriate and timely rather than premature, which helps create a sense of stability during a transition that often feels emotionally heavy.


Key Benefits of Hospice Care for Alzheimer’s Disease
Well-structured hospice care provides comfort that extends far beyond symptom management, since families receive emotional, educational, and practical support throughout the process. Patients benefit from a team that understands how Alzheimer’s affects communication, movement, appetite, and emotional regulation. Many caregivers discover that the right support team dramatically reduces stress by helping them understand which changes are normal and which require intervention.
- Medication oversight that focuses on comfort and reduces unnecessary prescriptions.
- Guidance for managing agitation, wandering, or other behavioral expressions.
- Emotional support for family members navigating grief before and after the loss.
- Consistent communication with nurses, aides, social workers, and chaplains who understand Alzheimer’s progression.
These advantages shape a calmer home environment where the patient can experience more peace in daily routines. Hospice care also empowers families to feel more confident while making decisions, especially once they understand that they are not alone in interpreting medical changes or caring for the patient’s evolving needs.
Common Signs That Alzheimer’s Has Reached Late Stage
Families often notice certain patterns that indicate hospice may be appropriate. These signs can be subtle at first, which leads many caregivers to postpone reaching out until the situation becomes overwhelming. Recognizing these indicators can help families take action sooner, giving the patient access to comfort-focused care at the right time.
1) Loss of verbal communication: Many patients speak only a few words or none at all, creating challenges in understanding pain or discomfort.
2) Significant personal care needs: Individuals may no longer be able to bathe, dress, or eat without full assistance.
3) Difficulty swallowing: This often leads to decreased food intake, weight loss, or choking concerns.
4) Frequent infections: Urinary tract infections, pneumonia, or other recurring illnesses become more common.
5) Reduced mobility: Patients may be unable to walk or may require assistance to change positions in bed.
These changes create a level of dependence that becomes difficult to manage without specialized support. Hospice teams work closely with families to create comfort-based routines, preventing unnecessary suffering by anticipating needs and reducing the emotional strain on caregivers.

Supporting Families in Louisiana, Mississippi, and New Mexico
Many families across these states care for loved ones with Alzheimer’s for years before considering hospice, often because they do not realize the level of support available. Local healthcare providers frequently refer patients to hospice once mobility, eating, or communication patterns change significantly. Medicaid programs in Louisiana, New Mexico, and Mississippi often cover hospice services for eligible Alzheimer’s patients, and this makes it easier for families to receive help without financial strain.
Community hospitals, primary care physicians, and memory care specialists regularly collaborate with hospice teams to create a smooth transition from active treatment to comfort-based support. Families frequently share that they wish they had reached out sooner because they did not realize how much guidance hospice could offer. By focusing on comfort rather than cure, hospice care lifts a weight off caregivers’ shoulders and allows them to focus on meaningful time with their loved one.
What Families Can Expect From the Care Team
Families receive coordinated support from a team that works together daily, sharing updates and adjusting the care plan as the patient’s condition evolves. The interdisciplinary nature of hospice ensures that no one person carries the burden of responsibility alone. This holistic approach becomes increasingly important as Alzheimer’s affects the patient’s physical, emotional, and cognitive wellbeing simultaneously.
- Nurses monitor symptoms and help maintain comfort.
- Aides assist with bathing, grooming, and repositioning.
- Social workers offer emotional guidance and connect families with community resources.
- Chaplains support spiritual or reflective needs based on the family’s beliefs.
Each role contributes to a comprehensive care plan that respects the patient’s needs while preparing the family for changes ahead. These layers of support allow families to step back from solely providing care and step forward into spending meaningful time with their loved one.
How Hospice Care Improves Quality of Life
Quality of life becomes the central priority once Alzheimer’s has progressed to late stage, which is why hospice emphasizes comfort, safety, and calm surroundings. Patients are supported through gentle routines tailored to their physical and cognitive capabilities. Caregivers often feel more at ease once the hospice team begins managing pain, behavioral shifts, and sleep patterns in a patient-centered way that reduces frustration for everyone involved.
Hospice professionals also teach families how to interpret subtle signs of discomfort or emotional distress, which equips them to respond more confidently. Personal care assistance, spiritual support, and regular nursing visits create a consistent environment that minimizes uncertainty. The focus remains on honoring the patient’s dignity while supporting the family through a deeply emotional chapter.


Why Specialized Alzheimer’s Hospice Care Matters
Specialized Alzheimer’s care ensures that the team understands how to communicate effectively, respond to nonverbal cues, and adjust routines that meet the patient where they are cognitively. This type of expertise creates a smoother, more peaceful environment because the care team anticipates challenges before they escalate. Families often describe a sense of relief once they realize the hospice team understands the small details that make daily care easier.
Such specialized knowledge also helps stabilize behaviors that might otherwise feel unpredictable or alarming. Predictable routines, thoughtful redirection strategies, and attentive symptom monitoring all contribute to a gentler care experience. Families gain confidence through this structure while retaining the reassurance that their loved one is receiving care that reflects dignity and compassion.
Choose Anvoi Hospice for Alzheimer’s Disease Care
Your family deserves support that combines expertise with warmth, especially when caring for someone living with Alzheimer’s disease. Anvoi Hospice provides specialized comfort-focused care that brings peace to patients and relief to caregivers during the most challenging stages. Our team understands the emotional weight of this journey and offers guidance that feels steady, patient, and reassuring. Contact Anvoi Hospice to learn how our compassionate Alzheimer’s care can help your family create calm, meaningful moments during this important time.








