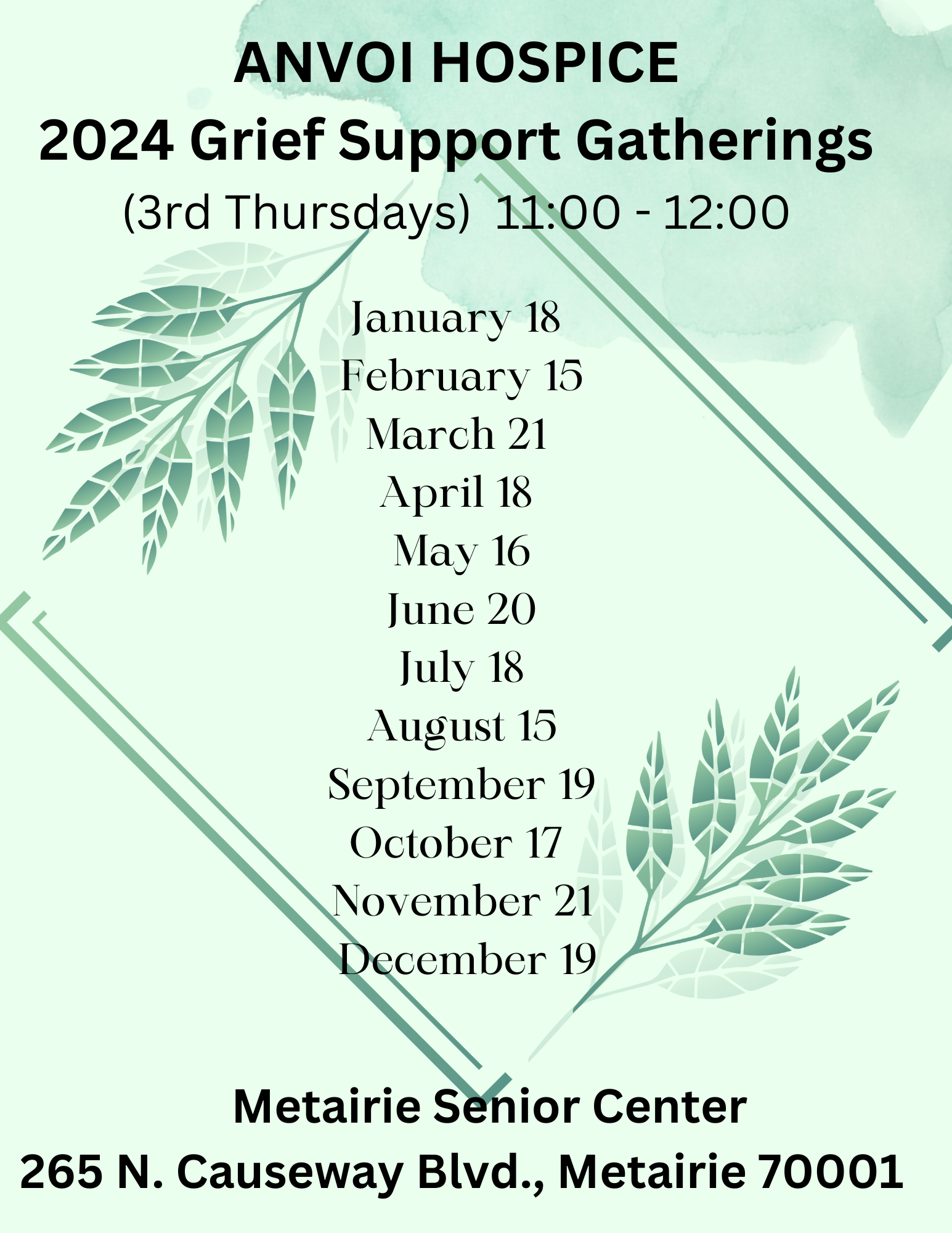
We host monthly grief support meetings. Click Here for 2024 Grief Support Gatherings.
Resources for Caregivers
Many families don’t know that they can receive additional specialized nursing care, medications, medical equipment, and supplies related to their loved one’s terminal illness at no cost much sooner than their loved ones’ final days.

3 Steps to Begin Care

Find Us
Visit our locations page to find a program near you. Call the location phone number 24-hours a day, 7-days a week. We'll help you learn about the process or schedule a no-obligation consultation.

Plan Ahead
Our admissions coordinator will promptly contact all responsible parties to plan consultations or patient assessments.

Get Care
Our admission team works directly with families and healthcare professionals to begin care. We bring hospice care to where the patient calls home, whether in a private home, nursing home or long-term care community.
Our Services
What We Provide
We genuinely care for our patients and his or her families. Each patient receives:
- Care wherever you call home
- Consistent weekly nurse visits
- Respite for caregiver relief
- Crisis care
- A unique personalized plan of care
- Bereavement and emotional support for 13 months
- Physician oversight
- 24 hours on-call nurse
- Volunteer program
- Medical equipment and supplies
- Medication for pain management and symptom control


When Should I Call Hospice?
You should call hospice if your loved one is experiencing any of the symptoms below:
- Frequent visits to the ER or hospital admissions
- A decline in his or her ability to perform daily tasks including eating, getting dressed, walking, or using the bathroom
- An increase in falls
- Changes to his or her mental abilities
- Progressive weight loss
- Skin tears, infections, and other signs of deteriorating health
Newsfeed

The Medicare Hospice Benefit is aimed at offering high-quality care during the final stages of life, without any cost to those on Medicare or their relatives.
READ MORE
Deciding when hospice is recommended can be difficult, especially when your loved one starts needing more comprehensive care.
READ MORE
Navigating the journey of end-of-life care can be overwhelming, especially when one is inundated with medical jargon and various options.
READ MORE
Navigating the final stage of life is a profound journey,....
READ MORE
Anvoi Health aims to provide practical advice and support for those facing the holidays after a loss, helping them to navigate this difficult period with greater ease and compassion.
READ MORE
Urinary tract infections, commonly abbreviated as UTIs, are infections that can affect any part of the urinary system.
READ MORE
In the realm of medical care, the terms 'hospice care' and 'palliative care' are often used interchangeably. However, while they share similarities, they also have distinct differences that are crucial to understand when considering the best care for you or your loved ones. Anvoi Health will demystify for you these two concepts, providing comprehensive insights into hospice vs. palliative care.
READ MORE
Many families wait to call hospice until the final days and weeks of his or her loved one's life not knowing they could have started receiving care at no cost much earlier.
READ MORE
Your hospice team is there to support you every step of the way, providing compassionate care and ensuring that your needs are met.
READ MORE
Hospice care can dramatically and positively impact quality of life. The goal is to empower the individual by providing knowledge and information to facilitate decision-making. Our staff consists of experts on pain control, symptom management, and emotional and spiritual comfort. Furthermore, our staff is committed to the education of patients and caregivers.
READ MORE
Our Anvoi Hospice pet-therapy dog provides a long list of mental health benefits. These canine encounters bring joy and reduce feelings of isolation, alienation, anxiety and depression. They help take a patient's mind off his or her aches and pains and encourage communication - including sharing stories and emotions.
READ MORE
Seeking hospice care early on at the end of life stage, allows patients and families to receive many different health benefits both physically, emotionally and spiritually.
READ MOREContact Us
Get In Touch With Us
Please do not include any personal health information in this form!




