CHECK OUT OUR CHILDREN'S BOOK FOR GRIEVING CHILDREN
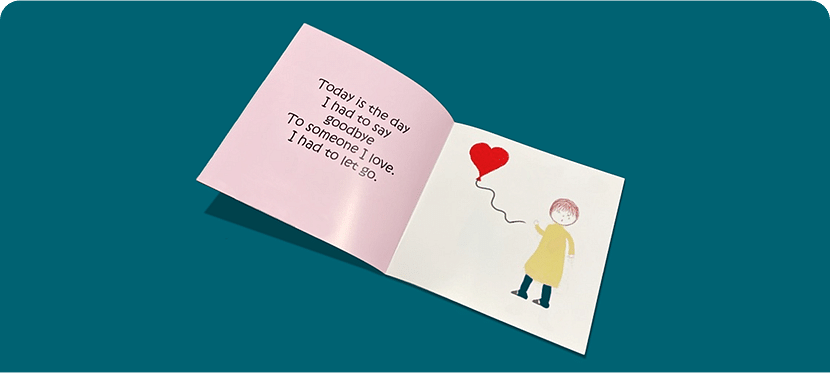
If you are interested in a free book on how to help children cope with the loss of a loved one please fill out the form below and someone from our team will reach out and send to you directly.
This form does not add you to a mailing list*

Frequently Asked Questions
Who pays for hospice? How do I know if it’s the right time for hospice? Find the answers to these questions and more.
A growing number of hospice programs have their own hospice facility or have arrangements with nursing homes, hospitals or inpatient residential centers that care for people who cannot be cared for at home. However, the cost to live in these settings may not be fully covered by your insurance, so it is best to find out if insurance covers this type of care before you call hospice.
Every person receiving hospice has access to a registered nurse, social worker, hospice aide, and chaplain (also known as the interdisciplinary team) and volunteers. The hospice team will work with you and your family to create a plan of care that will outline the actions and goals for your hospice care. All visits are based on you and your family’s needs in the care plan and your medical condition during the course of the illness. The frequency of volunteers and spiritual care is often dependent upon request and the availability of these services. Travel requirements and other factors may cause some variation in how many individuals each hospice staff serves.
The hospice team visits on an intermittent basis. This team includes physicians, nurses, social workers, hospice aides, chaplains and other specially trained care providers. The frequency of visits is determined by the patient’s needs. A hospice RN is on call 24 hours a day/7 days a week to answer questions and provide support. After hours visits are made as needed.
As the patient, it is your right, or the right of your decision maker, to determine when hospice care is right for you and which agency you would like to use. Others may recommend agencies for you to consider, but it is up to you to make the final decision. Not all hospice providers are the same, and it is important to receive the care that best fits your desires and needs.
You can stop hospice services at any time and for any reason. You can change your mind and resume aggressive treatment. Then if you wish to return to hospice care later, you can do so as long as you meet the medical hospice admission requirement.
Hospice makes the patient’s quality of life the focal point of care. Hospice professionals are trained to provide care and treatments that lessen the patient’s pain and other symptoms. Hospice strives to decrease the burden of medical treatment when such measures would not improve the patient’s quality of life. For some patients, this may mean decreasing the number of medications taken for chronic conditions.
Receiving hospice does not mean that death is imminent. Studies have shown that patients who elect hospice care earlier often live longer than those who continue to receive curative treatment. Hospice care is designed for patients who have a life expectancy of approximately six months or less. However, as long as the patient continues to meet hospice requirements, they may continue to receive services – even if this is longer than six months.
Urinary tract infections (UTIs) affect the urinary system, affecting the bladder and kidneys. They can be occasional inconveniences or recurrent nightmares. Anvoi provides information on why some individuals face repeated UTIs and how to reduce their frequency and manage symptoms.
Hospice services can be provided to a person who has a life-limiting illness wherever that person lives. This means a person living in a nursing facility or long-term care facility can receive specialized visits from hospice nurses, hospice aides, chaplains, social workers, and volunteers, in addition to other care and services provided by the nursing facility. The hospice and the nursing home will have a written agreement in place in order for the hospice to serve residents of the facility. The Medicare Hospice Benefit will cover the care related to your terminal illness, but it does not cover daily room and board charges of the facility. If you are eligible for Medicaid, Medicaid will cover room and board charges.
Many families wait to call hospice until the final days and weeks of their loved one’s life, not knowing they could have started receiving additional specialized nursing care and medications, medical equipment, and supplies related to their loved one’s terminal illness at no cost much earlier. Hospice care improves the patient’s quality of life by managing pain and other symptoms and improves the family/caregiver’s lives by having someone that they can lean on, seek guidance from and receive much-needed support during this difficult time.
Each person’s end-of-life experience is unique, as it is influenced by such factors as the specific illness, medications being taken, and the person’s overall health. In some cases, these changes may occur over a period of weeks; for others, the process lasts just a few days or hours.
However, a number of end-of-life changes are fairly common, as a person’s bodily functions naturally slow and stop. The following changes are often signs of this process, though not every patient exhibits all of these end-of-life signs.
• Less interest in eating or drinking. The person may only need enough liquid to keep his or her mouth from becoming too dry. How to help: Offer, but don’t force, food, liquids, and medication. In some instances, the person may no longer feel pain he or she had previously felt.
• Not passing fluids regularly. As bodily functions decline and the person eats and drinks less, their output of fluids will also decrease. How to help: Do nothing. However, if the patient is not passing fluids but feels the urge to do so, contact their nurse for advice.
• Speaking and moving less. Activity usually decreases significantly in one’s final days and hours. People may not respond to questions and show little interest in their surroundings.Hospice care may be considered for anyone doctors believe to have a life expectancy of less than six months. Usually at this point, active treatment aimed at recovery stops and hospice care is initiated. Hospice care focuses on producing the best possible quality of life in the patient’s remaining time.
Different diseases and conditions each have their own guidelines for hospice admission. The most common of these diseases or conditions include ALS, cancer, dementia, heart disease, HIV, kidney disease, liver disease, lung disease, Parkinson’s disease, stroke and coma. Sometimes a patient does not “fit” into the guidelines but still has a life expectancy of six months or less and therefore may be eligible for hospice.
In order to be eligible to elect hospice care under Medicare, an individual must be entitled to Part A of Medicare and certified as being terminally ill by a physician and having a prognosis of 6 months or less if the disease runs its normal course.• Medicare covers hospice care costs through the Medicare Hospice Benefit. See Medicare For More Info
• Veterans' Administration (VA) benefits also cover hospice care. See Va.gov For More Info
• The coverage of hospice care by Medicaid is optional and varies by state. See Medicaid For More InfoIn addition to Medicare and Medicaid, most private insurance plans, HMOs, and other managed care organizations recognize the value of hospice care and include hospice coverage in their plans. Additionally, some hospices provide charity care to patients who do not have insurance coverage or the ability to pay for their care.
Hospice redefines hope and helps patients and their families reclaim the spirit of life. Hospice care focuses on improving the patient’s quality of life allowing them to make the most of the time they have.
Palliative care is a specialized approach to medical care that focuses on improving the quality of life for individuals facing serious illnesses, regardless of whether those illnesses are considered curable or not. Learn more about palliative care.
Contact Us
Get In Touch With Us
Please do not include any personal health information in this form!











